CT SCAN OF ABDOMEN
- abdominal pain
- abdominal sepsis
- bowel obstruction
- postoperative complications
- trauma
- vascular compromise, e.g. aortic aneurysm
- CT Scan, MRI, EEG Films/Images with Reports.
- Blood for Serum Creatinine.
- FNAC/Biopsy Test Reports.
- Old Documents.
- Operation Note.
- Topogram
- Plain_ B31s medium smooth +_1.5 mm Abdomen
- I.V Contrast_ B31s medium smooth +_1.5 mm Abdomen
- Delay 5_Minutes_ B31s medium smooth +_1.5 mm Abdomen
CECT Abdomen/HBS 3-Phase /Upper Abdomen/Urogram/Abdomen angiogram or aortagram.
CECT Abdomen/HBS 3-Phase /upper
Abdomen/Urogram/Abdomen angiogram or aortagram.
CECT Abdomen/HBS 3-Phase
/upper Abdomen/Urogram/Abdomen angiogram or aortagram.
This is a basic article for medical students and other
non-radiologists
CT abdomen is an increasingly common investigation
that is used to help make diagnoses of a broad range of pathologies. A CT
abdomen in its simplest form is a CT from diaphragm to symphysis pubis
performed 60 seconds after pump-injection of iodinated contrast into a
peripheral vein. However, depending on the clinical question, a variety of
different protocols can be used.
Documents
1.
USG of Whole Abdomen/HBS/Upper
Abdomen/Pelvis/KUB.
2.
MRI Whole Abdomen/MRCP/HBS/ Upper
Abdomen/KUB/CT Urogram/ MR Urogram/IVU.
3.
Serum Creatinine Report.
4.
±Operation Note.
5.
History.
Preparation
1. খালি পেটে আসবেন (কন্ট্রাস্ট সিটি স্ক্যান এর জন্য)।
2. ২ লিটার পানির বোতল সাথে নিয়ে আসবেন।
3. পুরাতন কাগজপত্র সাথে নিয়ে আসবেন।
4.
সুতি কাপড় পড়ে আসবেন।
Indications
1.
Abdominal pain.
2.
Abdominal sepsis.
4.
Postoperative complications.
5.
Vascular compromise, e.g. aortic aneurysm.
6.
Infections such as appendicitis, pyelonephritis or
infected fluid collections, also known as abscesses.
7.
Inflammatory bowel disease such as ulcerative
colitis or crohn's disease, pancreatitis or
liver cirrhosis.
8.
Cancers of the liver, kidneys, pancreas,
ovaries and bladder as well as lymphoma.
10.
Abdominal aortic aneurysms (aaa),
injuries to abdominal organs such as the spleen, liver, kidneys, or other
internal organs in cases of trauma.
Important
pathology
1.
Bowel obstruction.
3.
Colon cancer.
4.
Intra-abdominal trauma.
Benefits
1.
Relatively quick and accessible.
2.
Reproducible findings.
3.
Complete assessment of the abdomen and
pelvis.
Limitations
1. Uses ionising radiation
a)
Risk of radiation-induced cancer.
b)
Approximately 100 times the dose of a chest
radiograph.
2. Requires iodinated IV contrast
a)
Risk of renal impairment.
b)
Risk of anaphylactic reaction.
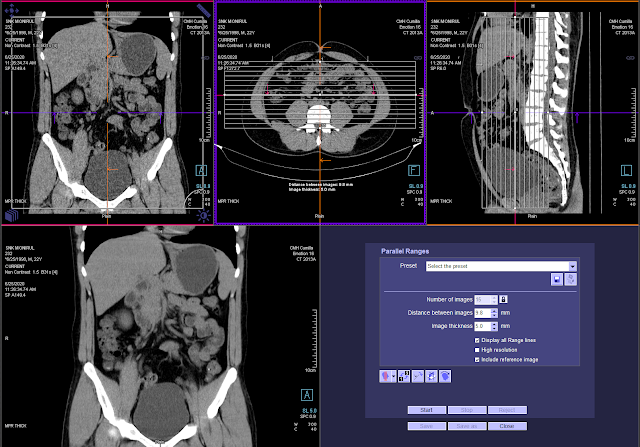
Procedure
1.
Check renal function.
2.
Lie patient supine on CT table.
3.
Scout image to plan study.
4.
I.V contrast injected via pump-injector.
5.
60-second delay.
6.
Scan from dome of diaphragms to symphysis
pubis.
Variations on a theme
Differing the IV contrast injection and timing may be
useful.
1. Dual-phase CT abdomen
a)
Two scans- non-contrast and arterial.
b)
Assessment of vascular supply and parenchyma.
2. 3-phase CT abdomen
a)
3-phase non-contrast, arterial and
porto-venous.
b)
Assessment of vascular supply and parenchyma.
Phases of enhancement
The purpose of
contrast-enhanced CT (CECT) is to find pathology by enhancing the contrast
between a lesion and the normal surrounding structures.
Sometimes a lesion will be hypo-vascular compared to the normal tissue and in
some cases a lesion will be hyper-vascular to the surrounding tissue in a
certain phase of enhancement.
So it is important to know in which phase a CT should be performed depending on
the pathology that you are looking for.
Scroll through
the images to see the enhancement in the different phases.
Non-enhanced
CT (NECT)
Helpful in detecting calcifications, fat in tumors, fat-stranding as seen in
inflammation like appendicitis, diverticulitis, omental infarction etc.
Early
arterial phase - 15-20 sec p.i. or immediately after
bolus-tracking. This is the phase when the contrast is still in the arteries
and has not enhanced the organs and other soft tissues.
Late
arterial phase - 35-40 sec p.i. or 15-20 sec after
bolus-tracking. Sometimes also called "arterial phase" or "early
venous portal phase", because some enhancement of the portal vein can be
seen. All structures that get their blood supply from the arteries will show
optimal enhancement.
Hepatic
or late portal phase - 70-80 sec p.i. or 50-60 sec after
bolus-tracking. Although hepatic phase is the most accurate term, most people
use the term "late portal phase". In this phase the liver parenchyma
enhances through blood supply by the portal vein and you should see already
some enhancement of the hepatic veins.
Nephrogenic
phase - 100 sec p.i. or 80 sec after bolus-tracking. This
is when all of the renal parenchyma including the medulla enhances. Only in
this phase you will be able to detect small renal cell carcinomas.
Delayed
phase - 6-10 minutes p.i. or 6-10 minutes after
bolus-tracking. Sometimes called "wash out phase" or
"equilibrium phase". There is wash out of contrast in all abdominal
structures except for fibrotic tissue, because fibrotic tissue has a poor late
wash out and will become relatively dense compared to normal tissue. This is
comparable to late enhancement of infarcted scar tissue in cardiac MRI.
Oral contrast
Oral contrast is given in
cases of suspected bowel perforation.
We use positive contrast: 1500
ml water with 50 cc non-ionic water soluable contrast.
Rectal contrast
Rectal contrast is given in
cases of suspected bowel perforation.
We use positive contrast: 1000
ml water with 30 cc non-ionic water soluable contrast.
Contraindication
1. Hypersensitivity to iodinated contrast
agent.
2.
Pregnancy.
3.
Irregular
rhythm.
4.
Renal
insufficiency (serum creatinine > 1.5 mg/ml). Kidney disease.
5.
Hyperthyroidism.
6.
Inability
to hold breath for 10 sec.
7.
History
of allergy to other medication.
8.
Metallic
interference (e.g: pacemaker, defibrillator wires).
9.
Excessive
radiation exposure.
10. Radioactive iodine treatment for thyroid disease.
Procedure (Bangla):
- প্রথমে
রোগীকে অল্প অল্প করে পানি খেয়ে প্রস্বাবের চাপ করতে বলি।
- প্রস্বাবের চাপ হলে Plain Scan নিই।
- Plain Scan নেওয়ার পর রোগীকে প্রস্বাব করে আসতে
বলি।
- প্যাথলজি Upper Abdomen এ থাকলে, ২ লিটার পানিতে
50 ml Inj, Iopamiro মিশিয়ে অল্প
অল্প করে ২ ঘন্টা ধরে ১.৫ লিটার পানি খাইতে বলি। রোগীর প্রস্বাবের চাপ হলে
আধা লিটার Oral Contrast মেশানো পানি খাওয়াইয়ে আই.ভি স্ক্যান নিই এবং ৫ মিনিট
Delay Scan নিই। রোগীর Oral Contrast রেকটামে পোঁছানো পর্যন্ত আনুমানিক ৪
ঘন্টার সময় একটা স্ক্যান নিই।
- প্যাথলজি lower Abdomen এ থাকলে, ১.৫ লিটার
পানিতে 50 ml Inj, Iopamiro মিশিয়ে
অল্প অল্প করে ২ ঘন্টা ধরে ১ লিটার পানি খাইতে বলি। রোগীর প্রস্বাবের চাপ হলে
১/২ লিটার Oral Contrast খাওয়াই এবং 500 ml Normal Saline with 15 cc contrast infusion set এর মাধ্যমে রেকটামে
প্রবেশ করাই। তারপর I.V Scan নিই এবং ৫ মিনিট Delay Scan নিই।
- পরীক্ষা শেষে,
রোগীকে স্বভাবিক খাবারের সাথে বেশি করে পানি খাইতে বলি।
7.
পরীক্ষা
চলাকালীন সময়ে রোগীর কোন প্রকার সমস্যা দেখা দিলে রেডিওলজিষ্টকে অবহতি করতে হবে । পরীক্ষা
পরবর্তী কোন সমস্যা হলে নিকটস্থ হাসপাতালের ইমার্জেন্সিতে যোগাযোগ করবেন।











0 Comments